Education
At NYU Grossman School of Medicine, our commitment to innovation has led us to bold new ways of bridging the gap between basic science research, medical education, and quality of patient care. With our Curriculum for the 21st Century, C21, we combine advances in learning strategies, emerging technologies, and informatics solutions to fulfill our trifold mission: to teach, to serve, and to discover.
Every student enrolled in our MD degree program receives a Full-Tuition Scholarship, regardless of merit or financial need, that covers the majority of the cost of attendance. Our Full-Tuition Scholarships make it possible for aspiring physicians to choose a specialty based on their talent and inclinations to better serve the communities who need it most, and to more easily pursue scientific breakthroughs that improve how we care for patients. We aim to turn the best and brightest future physicians into leaders with the potential to transform healthcare.
Our groundbreaking accelerated three-year MD program, launched in 2013, reduces the traditional medical school curriculum by one full year, with the ability to opt in during your first year of medical school. With our four- and five-year pathways to the MD degree, including dual degree programs, we offer unparalleled flexibility to customize your medical training in ways that align with your professional interests.
Join us in an educational experience that integrates clinical skills, quality, and evidence-based medicine, and emphasizes the importance of patient-centered care to inform and enhance healthcare in the 21st century.
Take a Virtual Tour

MD Admissions

Graduate Medical Education

MD/PhD Program

PhD Program

in quality and safety for inpatient and ambulatory care, Vizient, Inc.
medical school to offer Full-Tuition Scholarships for all students
specialties ranked in the top 10 nationally, U.S. News & World Report

Our approach to education is fueled by our commitment to diversity, innovation, and professional development.


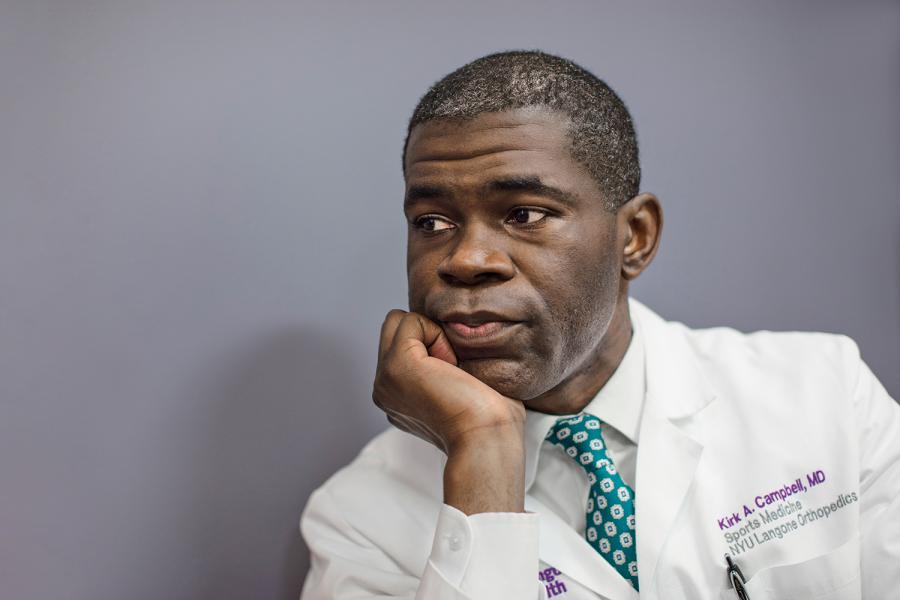
Diversity and Inclusion
We bring together a wide range of perspectives in order to foster excellence.

Innovation and Technology
We embrace the latest technological advances to enhance medical education.

Mentorship and Professional Development
We inspire the best and brightest to thrive in their careers.
Related News

‘Match Day’ Students Headed to Top Residency Programs

NYU Langone Ophthalmology Chair Receives Prestigious Award

Master’s Degree Program in Genome Health Analysis Launches

A $9.8 Million Gift Will Advance Pediatric Medicine
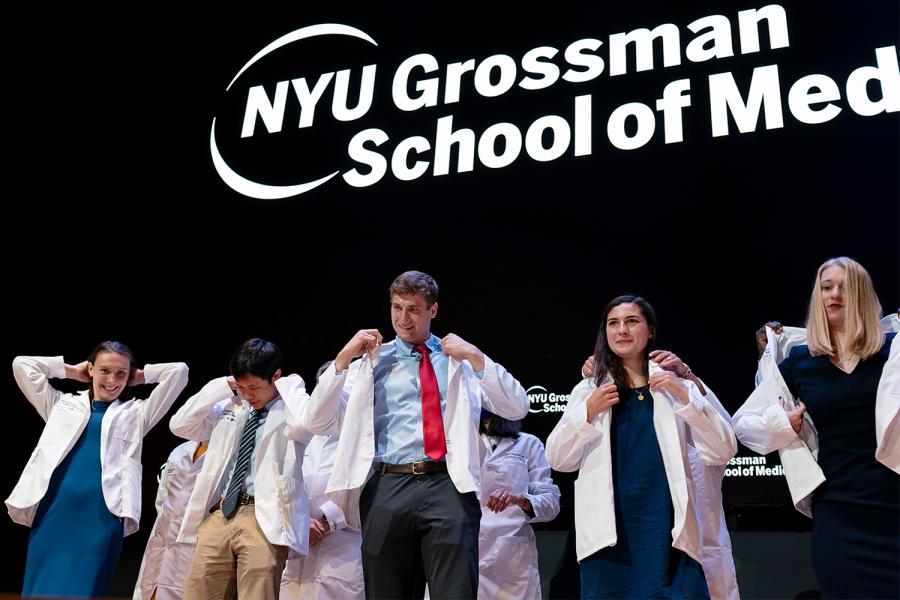
NYU Grossman School of Medicine Welcomes First-Year Students

Teleneurology Challenges Met by Training Curriculum

NYU Grossman School of Medicine Celebrates Class of 2023
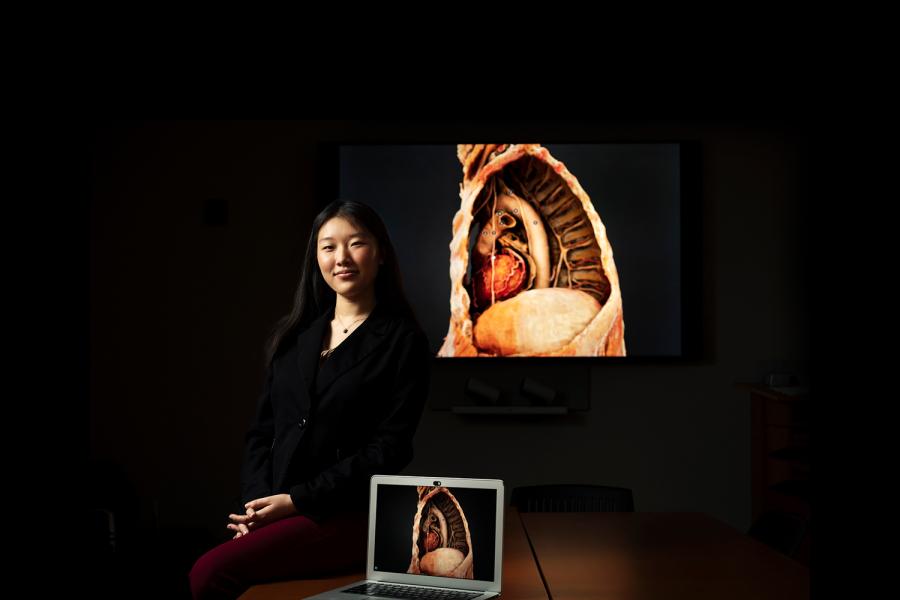
How AI Helps Students Learn to Become Better Doctors

NYU Grossman School of Medicine Students Celebrate Match Day

NYU Grossman School of Medicine Hosts White Coat Ceremony

New Vice Chair for Diversity, Equity & Inclusion Named